
Left Ventricular Assist Device (LVAD)
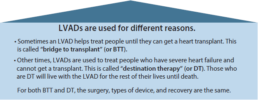
A device for patients with advanced heart failure.
You are being considered for an LVAD. This page is designed to help you understand what an LVAD is and to help you, your family, and your doctors think about what is best for you. Your values and goals are the most important factors in making a decision.
What is an LVAD ( Left Ventricular Assist Device)?
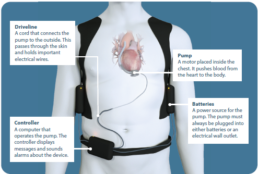
An LVAD is a mechanical device that helps your heart pump blood.
The video below features patients who have also faced this decision and provides more information about LVADs.
To read or print our booklet about this decision, Click Here.
Supporting Evidence
Here is a document outlining all evidence for practice decision aids, to help you in your decision.
